What to Expect
Convincing a loved one to enter treatment can be a difficult experience and you need to be aware of what to expect afterwards. An enormous amount of energy must be exerted by families and friends just to get them to the front door of the facility. What happens after they checks in?
Managing Insurance
Many families want or need to use their insurance to cover inpatient treatment, so they choose in-network facilities, which is the most cost-effective option. However, the length of treatment will be determined by the insurance company, not the person of concern, which can prevent patients from receiving the long-term rehabilitation they need. Although logic and empathy would show that the patient needs significant time to cover, insurance companies don’t always see it that way.
At an in-network facility, insurance only covers blocks of days. Typically, insurance plans cover an eight-day period of detox without any questions. After that initial block of time, the facility will request to extend the stay, in sequential blocks of 3-8 days, which insurance companies can authorize (or not). This can be a difficult thing for families to grasp. They know their loved one needs help, that he or she checked in for 28 days, but insurance companies will only pay for a limited period. Whenever possible, the family should maximize what insurance will pay for.
Without Full Coverage
In some cases, insurance companies will cover the full 28 days, but if that doesn’t happen, and insurance cuts off support, it can be a very difficult situation. It is likely that your loved one hasn’t had enough time to recover, so it becomes the responsibility of the patient or their family to pay for the remainder of treatment. Once the insurance company severs the funding, plans should be made for them to continue treatment in an outpatient setting.
Signing Releases
Checking into a rehabilitation facility can be a tedious process. It usually involves an in-depth medical analysis, a review of your insurance and associated costs, and preparation for detox. One concern shared by many people during this process is who has access to their medical information. This authorization is determined by a series of release forms that the patient can choose to sign or not. An adult who checks into treatment is fully in control of their own medical records.
There are different levels of release forms that must be signed. For instance, a patient may allow loved ones to call and verify that they are still present at the facility, as well as leave voice messages for them. In this case, the treatment center will generally call with weekly updates. Higher levels of release can include access to full medical records and routine consultations with care providers.
Getting Updates
Without a signed release form from the patient, the facility is not allowed to share any information to loved ones or anyone else who asks for it. This can be upsetting to family members, but it’s important to understand that the patient is still an autonomous being, regardless of their rehabilitation status.
Private conversations conducted in therapy are always kept private. Even if higher-level authorization forms are signed, many of the conversations held between families and care providers tend to be broad, centering on the patient, their challenges, and aftercare plans.
Take a Break
Getting someone into treatment can be a deeply stressful, taxing process. The days before and after a loved one steps through the front door tend to very emotional. After the person of concern enters treatment, I always tell their families to take a few days off to rest and relax. For the first time in a while, they don’t need to worry about their loved one, so they should focus on their own wellbeing and begin shifting their mindset from anxious overthinking to a positive outlook on the future.
Detox
Depending on the quantity and type of drugs and alcohol consumed in the days and weeks prior to treatment, you can expect your loved one will be in “detox”, a higher level of care, for a few days to a week. During the first few days, they will likely be heavily medicated and spending a lot of time sleeping, in no mood or shape to make phone calls. Detox can be a quiet period for all involved.
No News is Good News
When a loved one enters a treatment program, families often become worried, they want to know how things are going on the inside! Most families may feel disappointed with the level of communication provided by the treatment center, as most employ a no-news-is-good-news policy. However, you needn’t be too concerned. Treatment facilities are run by experts who know what they’re doing. You can expect a few calls per week updating you on your loved one’s progress if they’ve signed the consent form. However, you shouldn’t expect a daily call.
Patients may be allowed to call in the evening and on weekends. Try to keep those conversations as light as possible, if you can. Treatment is not the right time or place to bring them to account for the damage they’ve done.
The Call
At some point in early treatment, it is common to receive a phone call that can be summed up as “This place sucks, come get me.” Their dissatisfaction is often expressed in several different ways, relating to the food, their roommate, the therapist. There is always a complaint. Although it is important to acknowledge their claims, don’t jump into the hole with them. In the early days of recovery, they will go through many mood changes, and cycle through them quickly. Hear and respond to the complaint, but do not take immediate action. Call their therapist or another related staff member to express the concerns, so the facility can address the situation directly.
Family Programing
A good facility will have a program that includes the family by offering visits or video calls. These are important calls because aftercare as well as reintegration into the ‘real world’ will be discussed. Family members might still be hurt and processing experiences that occurred before treatment. So, the program is also a good time to work through feelings.
After treatment, change can happen at a rapid rate. This is sometimes unsettling, but the dynamic of the family will change for the better. Addressing buried emotions will free up emotional space and inspire families to believe in a brighter future.
Slow Weekends
The main staff at a facility is likely out of office during weekends. Weekends can feel a bit lonely in contrast to the busy weekdays and a patient’s emotions can be heightened. You will likely hear from your loved one during this time. Try to understand that time goes by slowly for them. They may need some extra loving support during these calls.
Setting up Aftercare
As soon as treatment begins, the family will need to put plans in place for continued care. If no changes are implemented after treatment, the chances of relapse increase significantly. The facility will speak to the recovering person about options. For most people, 28 days is barely enough time to establish a good treatment plan, so the facility will likely recommend extended care.
It’s important for the family to weigh their choices carefully by determining the most feasible option. This includes considering costs, previous commitments, and other criteria.
Discharge
Once treatment is complete, the recovering person will be discharged from the facility. For their first few days outside the treatment facility, they should be carefully monitored. It can be difficult to reintegrate into the family and reacclimatize to “normal life.” Leaving this environment might be very disorienting for them. The facility has become a safe space and returning to the outside world can be a jarring experience. Thus, it would be beneficial for someone to meet them at the facility and travel back home with them.
At this point, there should already be aftercare plans in place. At the treatment center, your loved one would have followed a strict schedule and built a strong support system. There will be a greater chance of successful recovery if the aftercare plan is implemented immediately after rehabilitation.
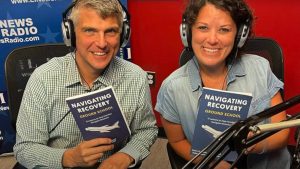
About Adam Banks
Adam Banks is a certified interventionist and the owner of Adam Banks Recovery. After receiving an MBA from the University of Chicago, Adam built a company acquired by United Health Care. His discipline and attention to detail comes from his former career as an airline pilot, holding an ATP, the FAA’s highest license.
Today, Adam is dedicated to helping others achieve long-term sobriety. His work has guided executives, pilots, and physicians on paths to recovery. Adam brings families together through a loving and inclusive approach.
Adam has authored four books on addiction. His recent work, Navigating Recovery Ground School: 12 Lessons to Help Families Navigate Recovery, educates families on the entire intervention process. He also offers a free video course for families considering an intervention for a loved one.
Adam is available for alcohol and drug intervention services in New York, Long Island, the Hamptons as well as nationally and internationally.