Families are frustrated and upset at the point they’re considering an intervention. What does an intervention look like? They would ask in their minds since they’ve tried everything to get a loved one to change. The days before making a call for an intervention are always hectic. It’s never an easy call to make and it always comes after being pushed over the proverbial edge.
Assessment
It’s natural that the first call feels a bit awkward. The person might be worried about privacy and trust. After all, they’ve contacted a stranger to share very personal and painful information about a loved one. However, the background story is integral to planning an intervention, so if you’re the one who places the call, you can expect questions like the following.
- How long has this behavior gone on for?
- Can you tell me about the last two weeks?
- Why do you feel that now is the time for an intervention?
- What substances do they use?
- Is there a mental health issue that you know about?
- Does the person have health insurance?
The assessment goes both ways. We encourage the caller to learn about interventions and the interventionist. Considering treatment or an intervention are major decisions that get made under pressure. During our assessment call, I teach callers about the process and what to expect.
Creating a Plan
Over the next few interactions, a plan will start to come together for the intervention. As I learn more about the person of concern, the right options for a treatment program become clear. We will consider the costs of the programs, location, insurance coverage, and find the right fit for the person. Inpatient treatment is not always the best course of action. We consider all options and what suits this individual and their family best.
Once a plan solidifies, the rest of the intervention process starts to fall into place.
Round up the Network
Prior to an intervention, families are worn out, angry, and in pieces. Ultimatums are being thrown around. Some people are at a loss, they just don’t know what to do anymore.
Rounding up the network and getting everyone on the same page is the most powerful part of an intervention. Finally, the family learns what to do, is in on the plan, and can constructively help the person of concern.
Long-term healing begins at this point. The family comes together in a unified way, maybe for the first time. We leave yelling and ultimatums behind as we shift into loving support.
The intervention
Most interventions don’t look like what you’d expect from seeing them on TV. Dropping in on someone and surprising him or her never goes well. People don’t react well to being cornered.
An intervention can be a very positive experience and it can happen many different ways.
Some interventions look easy. They might consist of a couple of phone calls to the person of concern. Some look more like family therapy, where a group comes together to begin a process of healing. The most influential people in an intervention are the family members, but it’s also paramount to have a moderator there. The moderator keeps the process positive as to avoid falling back into old patterns that don’t work.
I am finding now that people respond very well to Zoom interventions. Pre-pandemic, we wouldn’t have done a virtual intervention, but through experience we’ve found they are less confrontational to the person of concern. Another benefit is that family members who otherwise would not be able to join due to geographical limits are now able to be present. Even grandparents are well adapted to Zoom these days.
Treatment
There are many ways to get sober and not everyone should or needs to “go to rehab.” While going to a treatment center might be right for many people, there are other options, such as outpatient treatment, private therapy and psychiatry, medication routes, and 12-Step Meetings.
I tell families that an intervention will always spark change. Once the family is on board, the people that are healthy will shift how they interact with the person of concern. Family healing commences one way or another.
The path for the person of concern might not be going directly to rehab. They’ll often say no or want to try other options before going to inpatient treatment. No matter where they start their recovery, the most important thing is that there’s been a start.
More planning
Successfully entering a 28 day program is a great way to begin recovery, but it is just that, a beginning. Successful long-term recovery takes much more than 28 days. About three weeks into their inpatient program, plans need to be put in place for what happens next.
Consideration needs to be give to:
- An “after care program” that will continue treatment.
- The living situation, ie: can the person of concern live where they were before treatment?
- Evaluation of their home environment. Is it threatening to their recovery? Are there people who will negatively impact their success?
- Drug testing.
- Sober coaching and 12-step meetings.
This stage is fraught with emotion. Family members remember how the person was before the addiction took hold and the person of concern is now healthier and ready to make their own decisions. A safe reentry plan will take time to craft and the person of concern often takes some time to agree to it. Commonly, they feel they want to get home and “get on” with life, but putting a safe plan in place could be the difference between successful recovery and slipping back into old habits of using.
Long-term care
As the person of concern settles into their aftercare plan, they begin to stabilize. The individual might be remorseful or embarrassed as they begin to see the damage they left in their path. There is also a tension between the newly recovered person and their family. It was only 30 days ago that the family was taking care of an adult child. It’s natural the family isn’t convinced just yet that this time will be different.
Continuing therapy after rehab is very important. In the first 30 days after treatment, we want people to be busy doing recovery work, such as AA or IOP (intensive outpatient treatment).
I work closely with families during re-integration. The relapse rate is high the first few weeks out of treatment. By continuing family meetings, the family sees how this time is different and the person of concern can share their success and progress in a supportive atmosphere.
An intervention is not a one-off event; it is a recovery process. I commit to working with families for 90 days to ensure that the person suffering begins treatment successfully and has a plan that will ensure long term recovery. Committing the first time can lock in lasting recovery, making the intervention a process that only has to be done once.
About Adam Banks
Adam Banks is a certified interventionist and the owner of Adam Banks Recovery. After receiving an MBA from the University of Chicago, Adam built a company that was later acquired by United Health Care. His discipline and attention to detail comes from his former career as an airline pilot, holding an ATP, the FAA’s highest license.
Today, Adam is dedicated to helping others achieve long-term sobriety. His work has guided executives, pilots, and physicians on paths to recovery. Adam brings families together through a loving and inclusive approach.
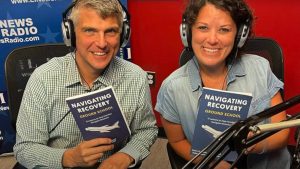
Adam has authored four books on addiction. His recent work, Navigating Recovery Ground School: 12 Lessons to Help Families Navigate Recovery, educates families on the entire intervention process. He also offers a free video course for families considering an intervention for a loved one.
Adam is available for alcohol and drug intervention services in New York, Long Island, the Hamptons as well as nationally and internationally.