Returning home from treatment marks a major milestone in the recovery process after treatment. Many changes will be made at home. Previously, there was a dynamic that allowed, and perhaps even supported, active addiction. Getting rid of all substances is only the beginning. Plans need to be put in place and strong boundaries erected to help re-shape familial relations.
The post-treatment period can be jarring for both the newly recovered person and their family. To some family members, it will be like their loved one got a vacation after causing so much turmoil. They are now leaving the people at home to pick up the pieces. On the other hand, the person who went to treatment will be filled with energy. Thus, eager to get back to their old life and fix the problem they’ve cause during their active addiction. Reintegrating the family can be difficult with challenges on both sides.
When planning for your loved ones return, I tell families to prepare for three options. Outstanding success, middle of the road, or no-change to behavior. I refer to these as options A, B and C.
Option A:
Option A is exciting and it’s what we all hope for. Addiction has begun to go into remission and the person of concern is actively participating in their own recovery. They are willingly taking suggestions and seeking addiction treatment such as IOP, 12-step meetings, and sober living options.
But even success has its fair share of challenges. The patient have had a month to undergo treatment and engage in meaningful self-reflection. They’ve become eager to get back to their families and resume their “normal lives.” However, their relatives, who didn’t spend a month away from everyday life, often have different sentiments. Spouses who had to manage household duties and childcare, as well as provide support for their intoxicated partner, are not swift to accept this new version of their loved one.
Before and during the period of intensive treatment, the spouse at home has been responsible for keeping the house in order and taking care of everyone on their own. Thus, when their partner returns and attempts to restructure the home environment, arguments can ensue.
The Tom and Sue Case Study
Take Tom and Sue, for example:
- Tom did great in treatment. He realized that he had abandoned his fatherly duties. Hence, upon returning home, wanted to make up for lost time. However, he and his wife, Sue, started getting into arguments over seemingly small things. While Sue desperately wanted a successful transition for Tom and their family, she was initially unprepared for it.
- In the past, Sue had to manage the household on her own for years due to her husband’s constant intoxication. In her eyes, she barely needed his support. So when he came back from treatment, ready to be “super-dad”, she grew very resentful. Tom would try to manage dinner but would make hamburgers on the night his wife always did tacos. He would want to take the kids on excursions, but his spontaneity would disrupt Sue’s structured plans. So friction at home became constant.
- Working with this couple to reintegrate back into their domestic lives took some time. Tom agreed to recovery work, such as IOP and daily breathalyzer tests. He realized that his family had suffered through his addiction for years. It would take time for him to earn back their trust. He also learned to ask where he was needed and offer his assistance, instead of taking the reins into his own hands.
- Both parties realized that the transition to normalcy needed to be taken slowly and that Tom’s recovery was top priority. Over the next six months, Tom did a lot of work to better himself through recovery programs and private therapy. Sue attended Al-Anon meetings to help herself cope with the transition.
We can see that Option A requires the patient’s full acknowledgement of wrongdoing and a strong desire to “do whatever it takes” to recover and mend their relationships.
Option B:
Option B is more difficult and can go both ways, success of failure. When the patient finishes treatment, it is recommended that they follow a structured program. But many people opt to do things their own way. This can create a feeling of dis-ease among family members.
Why?
They have no clarity on measuring the recovering person’s progress. The person can say they’re going to AA meetings, but the loved ones are doubtful because they cannot verify the claims. The plan has been weakened and no longer considers the family needs. It can’t also acknowledge how substance use or lack of recovery is affecting everyone.
To further support the person of concern, we clarify that a more intensive plan is required for successful recovery. Recovery contracts are a helpful tool for managing Option B. This is because clear expectations are set out in the case of relapse. They are not meant to be punitive but rather, an encouragement to undergo more treatment. If someone relapses, we double down on recovery by calling sponsors. Then we schedule more recovery meetings, encouraging a return to inpatient treatment.
With Option B, a return to use occurs, as relapse plays a role in most recovery stories. However, we want to address these relapses early, while the person of concern is remorseful and still wants recovery. They’re always willing to “double down” on the work suggested to stay clean and sober. In contrast, a relapse that goes on for days, or weeks, can unite patients and their families back to their starting point in a second.
Let’s look at Jack’s story:
- Jack’s marriage was on the verge of dissolution when he went into treatment. By the time his rehabilitation program had almost finished, he still hadn’t stabilized in the way we’d hoped. His wife, Dani, knew that if he came home right away, it would be trouble. She was used to managing the kids and was unwilling to take the risk of Jack coming back home and re-creating a chaotic environment.
- Jack reluctantly went into Sober Living, and quickly relapsed. After a weekend of binge drinking, he went back to a rehabilitation facility for another two weeks of inpatient treatment. He also agreed to an intensive aftercare program. This fast-acting approach addressed Jack’s relapse quickly and helped him return to a structured recovery plan. Sometimes, a relapse is necessary because it allows the patient to clearly see the destruction caused by their substance use and motivate them to dedicate themselves to recovery.
When someone is in treatment, I spend a lot of time talking to their families about Option B. Addiction was controlling the family prior to treatment. However, they can now decide how the addiction is going to be managed going forward. We never want to see families get sucked back into the vortex of addiction. They must be managers of the recovery process.
Option C:
Option C is the easiest for families to manage because it is what they have become familiar with. The person of concern would have shown no signs of change and we will have returned to the starting point. We tell families to prepare for this in a concrete way. If this option becomes reality, what are the consequences? Does this option mean divorce or limited interaction with children? Will housing and/or financial support be affected?
Even in the scenario of Option C, we never want families to submit to the addiction. To avoid being controlled by it once again, family members must ask themselves the hard questions. Can I live alone? Do I need this person? Can the person of concern live elsewhere? Am I reliant on them financially? Can someone else assist with childcare?
I’ve had families take out a sheet of paper and consider the potential consequences of detaching from the patient. We work together to create a financial plan and discuss housing, schooling, and childcare options to determine whether the family will be secure without their loved one.
This step is not meant to punish the person of concern, but, offer protection and control to their relatives. Our hope is that families never need that white sheet of paper, but it’s always better to go into a situation knowing that you have a plan of action and can regain control at any time. Going through options A, B and C prepare families for whatever comes next and removes the addiction from the driver’s seat. You will never need to be subservient to the addiction again.
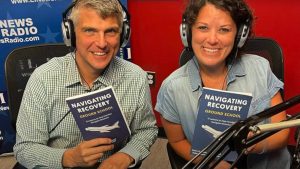
About Adam Banks
Adam Banks is a certified interventionist and the owner of Adam Banks Recovery. After receiving an MBA from the University of Chicago, Adam built a company that was later acquired by United Health Care. His discipline and attention to detail comes from his former career as an airline pilot, holding an ATP, the FAA’s highest license.
Today, Adam is dedicated to helping others achieve long-term sobriety. His work has guided executives, pilots, and physicians on paths to recovery. Adam brings families together through a loving and inclusive approach.
Adam has authored four books on addiction. His recent work, Navigating Recovery Ground School: 12 Lessons to Help Families Navigate Recovery, educates families on the entire intervention process. He also offers a free video course for families considering an intervention for a loved one.
Adam is available for alcohol and drug intervention services in New York, Long Island, the Hamptons as well as nationally and internationally.